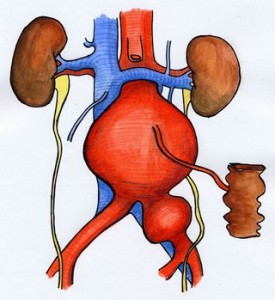
The traditional operation involves cutting open your abdomen to replace the aneurysm with an artificial piece of artery (a graft). This is a major operation and carries some risk. However, it is successful in most cases and the long term outlook is good. The graft usually works well for the rest of your life.
Recovery and aftercare
You will usually spend 1-2 days in the Intensive Care or High Dependency Unit after your operation so that your progress can be closely monitored.
It is usually necessary for you to remain on a breathing machine for a short period after the operation but you will be taken off this as soon as possible.
Following this sort of surgery, the bowel stops working for a while and you will be given all the fluids you require in a drip until your bowel can cope with fluids by mouth.
It may be necessary for you to have a blood transfusion. Some hospitals recycle your own blood lost during the operation and give it back to you.
The nurses and doctors will try and keep you free of pain by giving painkillers by injection, via the epidural tube in your back, or by a machine that you are able to control yourself by pressing a button.
Over the next few days as you start to recover, the various tubes will be removed and you will return to the normal ward until you are fit enough to go home (usually 8-10 days after the operation).
You will be given a small injection every day to lower your chance of getting a deep vein thrombosis (DVT) or pulmonary embolus (PE) after the operation. These will continue until you are fully mobile and discharged from hospital.
Going home and aftercare
If your stitches or clips are the type that need removing this is usually done whilst you are still in hospital. If not, it will be arranged for your GP’s practice or district nurse to remove them and check your wound. 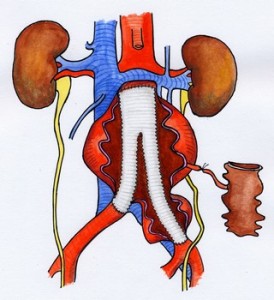 You will feel tired for many weeks after the operation but this will improve as time goes by.
You will feel tired for many weeks after the operation but this will improve as time goes by.
Exercise: Regular exercise such as a short walk combined with rest is recommended for the first few weeks followed by a gradual return to normal activity.
Driving: You will be able to drive when you can perform an emergency stop safely. This will normally be 3-4 weeks after surgery, but if in doubt check with your own doctor. You should inform your insurers that you have undergone major surgery.
Bathing: Once your wound is dry you may bathe or shower as normal. This will normally be before you leave hospital.
Work: If this applies to you, you should be able to return to work within 6-12 weeks of surgery. Your GP will advise you of this when you see him/her for your sick-note.
Lifting: You should avoid heavy lifting or straining for 6 weeks after the operation.
Medicines: You will usually be sent home on a small dose of aspirin and a statin if you were not already taking them. This makes the blood less sticky and reduces your cholesterol levels. If you are allergic to aspirin, or if it upsets your tummy, an alternative drug may be prescribed.
Complications
As with any major operation there is a small risk of you having a medical complication such as:
- Heart attack
- Stroke
- Kidney failure
- Chest problem
- Loss of circulation in the legs or bowel
- Infection in the artificial artery
Each of these are rare, but overall it does mean that some patients may not survive their operation or the immediate post-operative period.
For most patients this risk is about 7% from an open aneurysm repair - in other words 93 in every 100 patients will make a full recovery from the operation.
The doctors and nurses will try to prevent these complications and to deal with them rapidly if they occur. Surgeons at your hospital will be able to tell you the local death rate for this operation.
If your risk of a major complication is higher than this, usually because you already have a serious medical problem, your surgeon will discuss this with you. It is important to remember that your surgeon will only recommend treatment for your aneurysm if he or she believes that the risk of the aneurysm bursting is much higher than the threat posed by the operation.
DVT/PE: After any large operation there is a risk of DVT (Deep Vein Thrombosis) or PE (Pulmonary Embolism). You will be on medication to reduce the risk, but this cannot be completely negated. If you do get a DVT or PE you will require a period of tablets (Warfarin) to thin the blood for 3 to 6 months.
Chest infections: These can occur following this type of surgery, particularly in smokers, and may require treatment with antibiotics and physiotherapy.
Wound infection: Wounds sometimes become infected and this may need treatment with antibiotics. Serious infections are rare. Occasionally, the incision may need to be cleaned out under anaesthetic.
Graft infection: Very rarely (about 1 in 500), the Dacron graft may become infected. This is a serious complication, and usually treatment involves removal of the graft.
Fluid leak from wound: Occasionally the wound in your groin can fill with a fluid called lymph that may leak between the stitches. This usually settles down with time.
Bowel problems: Occasionally the bowel is slow to start working again after the operation. This requires patience and fluids will be provided in a drip until your bowels get back to normal.
Sexual activity (Impotence): This may occur in men due to nerves in your tummy being unavoidably cut during the operation. This occurs in about 10% of patients.
What can I do to help myself?
If you are a smoker you should make a determined effort to stop completely. Continued smoking will cause further damage to your arteries and increases the risks of heart attacks, strokes, and problems with the circulation in your legs.
General health measures such as reducing weight, a low fat diet and regular exercise are also important.
More information and advice about vascular health.
Whilst we make every effort to ensure that the information contained on this site is accurate, it is not a substitute for medical advice or treatment, and the Circulation Foundation recommends consultation with your doctor or health care professional.
The Circulation Foundation cannot accept liability for any loss or damage resulting from any inaccuracy in this information or third party information such as information on websites to which we link.
The information provided is intended to support patients, not provide personal medical advice.